Definition
Mammography is a specific type of imaging that uses a low-dose x-ray system to examine the breasts.
A mammography exam, called a mammogram, is used to aid in the early detection and diagnosis of breast diseases in women by looking for abnormalities, or problems, with a woman’s breasts. The test uses a special x-ray machine to take pictures of both breasts. The results are recorded on film and interpreted by a specialist radiologist.
Mammograms look for breast lumps and changes in breast tissue that may develop into problems over time. They can find small lumps or growths that are impossible to feel. Breast lumps or growths can be benign (not cancer) or malignant (cancer). If a lump is found, the radiologist may suggest a biopsy, a test where a small amount of tissue is taken from the lump and area around the lump. A pathologist (specialist doctor) looks at the sample under the microscope to see if there is any sign of cancerous cells.
Finding breast cancer early means that a woman has a better chance of surviving the disease. There are also more choices for treatment when breast cancer is found early.
Book Appointment
How the test is performed
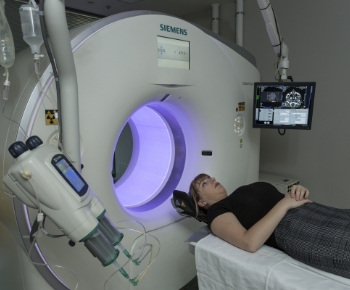
During mammography, a specially qualified radiographer will position your breast in the mammography unit. Your breast will be placed on a special platform and compressed with a paddle (often made of clear Plexiglas or other plastic). The radiographer will gradually compress your breast.
Breast compression is necessary in order to:
Even out the breast thickness so that all of the tissue can be visualised.
Spread out the tissue so that small abnormalities are less likely to be obscured by overlying breast tissue
Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged
Hold the breast still in order to minimise blurring of the image caused by motion
Reduce x-ray scatter to increase sharpness of the image.
You will be asked to change positions between images. The routine views are a top-to-bottom view and an angled side view. The process will be repeated for the other breast.
You must hold very still and may be asked to keep from breathing for a few seconds while the x-ray image is taken to reduce the possibility of a blurred image. The radiographer will walk behind a clear lead glass screen to activate the x-ray machine.
When the examination is complete, you will be asked to wait until the radiologist determines that all the necessary images have been obtained.
The examination process should take about 30 minutes.

Is a mammogram safe?
A mammogram is a safe, low-dose x-ray of the breast. A high-quality mammogram, along with clinical breast examination (exam done by a doctor) are the most effective tools for detecting breast cancer early.
How is a mammogram done in a woman with breast implants?
If you have breast implants, be sure to tell your radiographer. You will need a radiographer who is trained in x-raying patients with implants. This is important because breast implants can hide some breast tissue, which could make if difficult for the radiologist to see breast cancer when looking at your mammograms. For this reason, to take a mammogram of a breast with an implant, the radiography might gently lift the breast tissue slightly away from the implant.
You will also require a longer appointment time for the procedure.
How often should I get a mammogram?
Australian recommendations are to have a mammogram once every two years starting age 50. Women at increased risk of breast cancer can start screening mammography earlier, often at age 40. Talk to your doctor about how often you should have a mammogram. Be aware that mammograms don’t take the place of having a physical examination from your GP.
If you find a lump or see changes in your breast, talk to your GP right away no matter what your age. Your GP may order a mammogram or ultrasound, or refer you to a surgeon for further evaluation.

How to prepare for the test
Do not schedule your mammogram for the week before your period if your breasts are usually tender during this time. The best time for a mammogram is one week following your period. Always inform your doctor or radiographer if there is any possibility that you are pregnant.
We also recommend that you:
Do not wear deodorant, talcum powder or lotion under your arms or on your breasts on the day of the exam. These can appear on the mammogram as calcium spots.
Describe any breast symptoms or problems to the radiographer performing the exam. If possible, obtain prior mammograms and make them available to the radiologist at the time of the current exam.
Ask when your results will be available; do not assume the results are normal if you do not hear from your doctor or the mammography facility.
How the test will feel
You will feel pressure on your breast as it is squeezed by the compression paddle. Some women with sensitive breasts may experience discomfort. If this is the case, schedule the procedure when your breasts are least tender. Be sure to inform the radiographer if pain occurs as compression is increased. If discomfort is significant, less compression will be used.

Why the test is performed
Mammograms are used as a screening tool to detect early breast cancer in women experiencing no symptoms. It can also be used to detect and diagnose breast disease in women experiencing symptoms such as a lump, pain or nipple discharge.
What are the Benefits vs the Risks?
Benefits
Imaging of the breast improves a physician’s ability to detect small tumours. When cancers are small, the woman has more treatment options and a cure is more likely.
The use of screening mammography increases the detection of small abnormal tissue growths confined to the milk ducts in the breast, called ductal carcinoma in situ (DCIS). These early tumours cannot harm patients if they are removed at this stage and mammography is the only proven method to reliably detect these tumours. It is also useful for detecting all types of breast cancer, including invasive ductal and invasive lobular cancer.
No radiation remains in a patient’s body after an x-ray examination.
X-rays usually have no side effects in this diagnostic range.
Risks
There is always a slight chance of cancer from excessive exposure to ionising radiation. However, the benefit of an accurate diagnosis far outweighs the risk.
The effective radiation dose for this procedure varies. See the Safety page (www.RadiologyInfo.org/en/safety/) for more information about radiation dose.
As with any medical test, mammograms can have limits. These limits include:
False negatives can happen. This means everything may look normal, but cancer is actually present. False negatives don’t happen often. Younger women are more likely to have a false negative mammogram than are older women. This is because the breast tissue is denser, making cancer harder to spot.
False positives can happen. This is when the mammogram results look like cancer is present, even though it is not. False positives are more common in younger women than older women.
Mammograms are only part of a complete breast examination. At DiagnostiCare we recommend and perform breast ultrasound to give a thorough and comprehensive view of the breast tissue.
Women should always inform their physician or radiographer if there is any possibility that they are pregnant. See the Safety page (www.RadiologyInfo.org/en/safety/) for more information about pregnancy and x-rays.

A word about minimising ionising radiation exposure
Special care is taken during x-ray examinations to use the lowest radiation dose possible while producing the best images for evaluation. National and international radiology protection councils continually review and update the technique standards used by radiology professionals.
State-of-the-art x-ray systems have tightly controlled x-ray beams with significant filtration and dose control methods to minimize stray or scatter radiation. This ensures that those parts of a patient’s body not being imaged receive minimal radiation exposure.




Book your appointment online or call now 03 9337 8288
Book AppointmentFrom the moment you request an appointment to the final referral, we aim to make your experience as smooth and comfortable as possible. Here is our working process for all DiagnostiCare patients.
-

Request Appointment
-

Patient Examination
-
Results To Referrer



-
Use of low-radiation techniques for safety.
-
Capable of performing complex imaging procedures.
-
Bulk-billing available for eligible patients.
-
Strong commitment to patient privacy and confidentiality.
-
Offering both walk-in and appointment-based services.
-
Equipped with the latest 3D imaging technology.
-
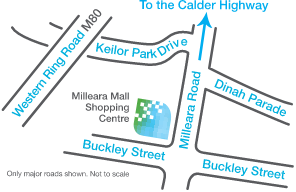
Suite 46 Level 1 Milleara Mall,
235 Milleara Road East Keilor VIC 3033 -
Monday - Friday 8.00am - 6.00pm Saturday 8.00am - 1.00pm